Issue # 15: In with the SCORTCH and out with the TORCH!
Rethinking TORCH infections// 5 Q & As with an experienced NICU nurse
How are you all doing this late November? Crazy the year is almost over! Let’s talk about TORCH infections today.
Penner et al. published the above article in 2020, in which they suggested we should change the commonly used acronym to ‘SCORTCH’ infections. This would, they argued, put a greater emphasis on syphilis and CMV, both diseases we see commonly in the NICU.
Before we get to syphilis, let’s talk about Cytomegalovirus (CMV) for a second. If you’ve worked in the NICU or nursery at all, you’ve probably taken care of a baby with CMV.
Maybe you had a feeder-grower who became lethargic and started having more events. You performed a sepsis screen: the platelets were low, but there was no significant left shift and the culture remained negative. You sent a CMV PCR and lo and behold it came back positive. Not surprising! CMV is the most common congenital infection (passed through the placenta, vaginal secretions or through breast milk). Check out this info-graphic from the National CMV foundation:
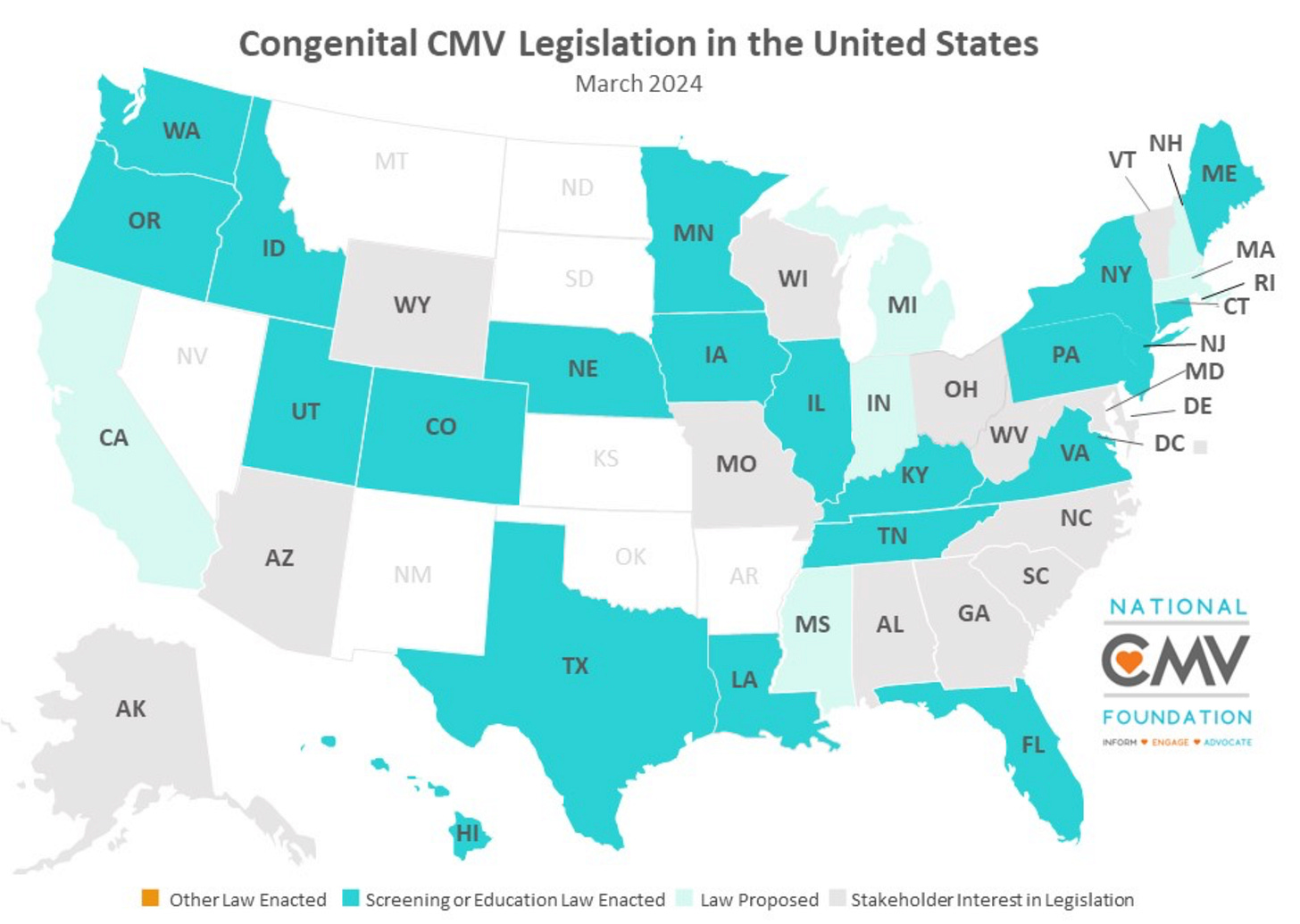
Or you have a newborn who failed their hearing screen, and per your state’s law, you sent a CMV test (here we send a PCR on saliva) and it came back positive. Not every state has required CMV screening yet, though. The map below shows the current legislation per state in the US. Basically, though, there’s a lot of CMV everywhere!
So maybe, the new acronym should be CROTCHeS? Eewww. (Many of the infections are sexually transmitted, so could serve as a double reminder?) But, ewww.
Also, we do have the little issue of syphilis exploding in the last decade. We don’t want that S tucked away at the end of the acronym. Check out this graph from the CDC:
Look at those blue columns which represent the cases of congenital syphilis per year. The prevalence has increased by a shocking 10 times since 2012. Most of these cases, per the CDC, could have been prevented if we treated mothers appropriately after the diagnosis was made (31%), provided adequate prenatal care (28%) or identified seropositive mothers in time for treatment (11%).
But it’s not all doom and gloom! Peek again at the chart above: the rate of increase in cases of congenital syphilis has slowed down. AND! 2023 was the fist year the rate of primary and secondary syphilis (the straight black line) actually went down!!!
So- talk with your OB colleagues, your mothers in newborn and the NICU. We can make progress together! Still though, with these sorts of rates of syphilis and CMV, you can see why the acronym SCORTCH makes sense!
Our last video was on these TORCH/ SCORTCH infections.
Watch it here, if you haven’t seen it yet.
If you’d like a worksheet on topics covered by our videos (and lots of other perks- including debriefing videos), then sign up for our YouTube membership here: JOIN
Here is the PDF summary of the video:
And a few MCQs on TORCH infections:
Five Questions with….
I met Anne Shields (NICU RN, RNC NNIC AND ELBW) through YouTube – and from very early on she became the ideal friend! Always encouraging us, coming up with new ideas, and offering her own perspective. I love hearing from people who have worked in the NICU for a long time- and still LOVE their jobs, so I was overjoyed when she agreed to answer 5 questions for this newsletter.
Briefly, Anne graduated from Penn State in 1991 and has worked as a nurse since then, starting in the mother-baby unit, then L and D before moving to the NICU. For several years, she worked as a travel nurse all over the US, but has since settled down in her current role in San Jose. So here goes, 5 questions for the lovely Anne:
What is your favorite aspect of being a NICU nurse?
My favorite part is getting to know the families and being able to teach them about their babies. I love getting the scared dads to hold their babies skin-to-skin for the first time.
What would you say has changed the most about the NICU since you started?
So much has changed. When I started it was a "get in, get out" culture. Skin-to skin time was limited. The Oscillator was a stiff tube, so it needed a "pancake flip" to turn the baby. A development boundary was a rolled blanket that was not very stiff. Mixing meds and drips has changed so much! There are so many more examples, but the field has definitely grown since I started.
Any practical advice on how to deal with difficult situations? Sad colleagues? Angry parents?
For sad colleagues, I give them a hug. For parents, I usually go overboard explaining everything I do. I mean, I go all in with nursing lectures, talking to them for a very long time. I'll give them videos to watch, booklets to read. I think parents get frustrated because they want more info on their baby’s situation or on what they can do.
What advice would you give to someone who just started as a NICU nurse?
New nurses: don't stop learning. If you’ve never had to take care of a baby with a chest tube, read about it and imagine what you would do. Jump in. Do something if there is an admit. Don't take a lot of request days! Read about your baby's issues! Think!
How have you managed to avoid burn-out? Any life tricks?
Previously, I avoided burn-out by being a travel nurse. You’re not anywhere long enough to feel the politics. Now, I plan vacations. Find your group at work and make their shifts great, they will start doing things for you too.
Bonus question: What can you not live without in the NICU?
The straws to draw up milk and the tiny straws to drip milk on their lips. Breast milk warmers!
We hope you’re enjoying this newsletter as much as we enjoy writing it. We’d love to hear your thoughts either way…(Podcasts you’re listening to? Items you can’t live without? Want to be on our 5 questions segment?!)
Stay healthy, and we’ll be back in your inboxes in 2 weeks,
Tala and Arianna











YES! Feel same way about you Karen :)
a newborn of 31 weeks 1440g, born naturally, mother states that he grew less in the end, head circumference on P15 (27 cm), weight on P50 and length on P75 (44 cm), IP=1.69; should I think the cause is a placental anomaly or a TORCH infection?